Emergency Federal legislation relaxes Medicare requirements for telehealth services to combat COVID-19
On March 6, 2020, the President signed into law the Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020 (H.R. 6074, the “Act”), bi-partisan legislation that promotes telehealth services for Medicare patients and provides additional emergency funding for fiscal year 2020 to combat the ever-increasing spread of the coronavirus (COVID-19) at the federal, state and local levels.
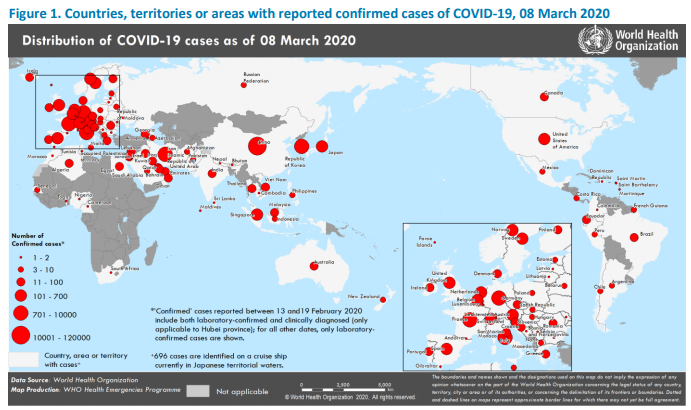
As of March 8, 2020, there have been 213 confirmed and/or presumed positive cases of COVID-19 in the United States, including 11 deaths. According to the World Health Organization (WHO), globally as of March 8, 2020, there are 105,586 confirmed cases of COVID-19, with 3,584 deaths (3,100 in China alone). Figure 1, reproduced from the WHO COVID-19 Situation Report – 48, depicts the locations where confirmed cases have been reported. Given the rapid pace in which the confirmed cases are increasing, the WHO’s website has a section dedicated to the COVID-19 outbreak that is updated on a daily basis.
The Act, which was fast-tracked through both houses of Congress and the President in a mere 2-days, provides for $8.3 billion in emergency funds to be allocated to various agencies within the Federal Department of Health & Human Services (HHS), including the Food and Drug Administration (FDA), the Centers for Disease Control and Prevention (CDC) and the National Institutes of Health (NIH). The Act also provides emergency supplemental appropriations to the Small Business Administration (SBA), the Department of State and the US Agency for International Development for activities related to combatting the COVID-19.
More notably, however, Division B, entitled the Telehealth Services During Certain Emergency Periods Act of 2020, grants the Secretary of HHS authority to waive the requirements of telehealth services to Medicare beneficiaries in an “emergency area” during an “emergency period.”
Generally, telehealth services to Medicare beneficiaries is only reimbursable upon meeting the following requirements:
- The beneficiary is located in a qualifying area (county outside a Metropolitan Statistical Area (“MSA”) or Rural area);
- With limited exceptions, the beneficiary receives telehealth services at an originating site;
- The telehealth services are provided by a qualified provider;
- The qualified distant site practitioner renders his/her services from a distant site;
- The services provided are among the identified CPT Codes for telehealth services (which includes office and out-patient visits); and
- The communication must be through an interactive audio and video telecommunication system that utilizes real-time communication.[1]
However, the Act allows the Secretary to waive the “originating site” requirement and the communication device requirement, allowing, instead, for telehealth consultations between the provider and patient to take place while the patient is in his/her home and may utilize his/her smartphone if it has audio-video communication capabilities. While the use of one’s smartphone in the comfort of one’s own home is a step forward in the Medicare telehealth arena, providers must still be cognizant of any applicable state limitations, such as licensing, scope of practice and cross-border restrictions for telehealth services.
If you have any questions about this alert, please contact the author or your Butzel Long attorney for assistance.
Debra A. Geroux, JD, CHC, CHPC
248.258.2603
geroux@butzel.com
[1] See 42 USC § 1834(m)